Pattern of Refractive Errors Amongst Children Attending a New Teaching Hospital in Kaduna, Nigeria: A 2‑Year Review
DOI:
https://doi.org/10.60787/jmwan-v7i1-35Keywords:
visual acuity, uncorrected refractive error, refractive error, Kaduna, children, Asthenopic symptomsAbstract
AIM: The aim of this study was to assess the prevalence and pattern of presentation of refractive errors (REs) amongst children 5–16 years who attended the eye clinic of a tertiary hospital over a 2‑year period.
SETTING: The outpatient unit of the Department of Ophthalmology, Barau Dikko Teaching Hospital, Kaduna, Nigeria.
SUBJECTS AND METHODS: A descriptive retrospective study of children aged 5–16 years, who presented to our facility between January 2017 and December 2018 with various ocular complaints. Those with presenting visual acuity <6/9 were included in the study. Demographic data were retrieved from patient records. The visual acuity, ocular complaints, RE, general ocular examination and prior
history of spectacles use were also extracted from the records. Statistical analysis was done with SPSS version 18.
RESULTS: A total number of 14,004 patients of all ages where seen in outpatients Department of Ophthalmology Clinic. Five thousand six hundred and nine were children aged 5–16 years. Seven per cent of the patients (392) had REs, while 93% (5217) had no RE. The mean age was 10.7 years and with a male‑to‑female ratio of 1.2:1. Two hundred and thirty patients were in the 11–16 years (58.6%),
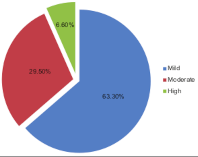
while 162 (41.4%) belonged to the 5–10 years age group. Myopia accounted for 212 (54%), while mixed astigmatism only 9 (2%). Hyperopia 100 (27%), simple myopic astigmatism 40 (10%), compound myopic astigmatism 18 (4%) and compound hyperopic astigmatism 13 (3%) made up the other REs. Asthenopic symptoms accounted for 78% of all presenting ocular symptoms and were
common amongst those with myopia and astigmatism, while 22% had no symptoms. Most of the REs were of mild‑to‑moderate grade based on their spherical equivalent.
CONCLUSION: RE was identified as a problem amongst children 5–16 years with myopia more common. Most cases of RE in this study were myopia and associated with ocular complaints which were mostly asthenopic symptoms. The majority of the REs were mild to moderate.
Downloads
References
Dandona R, Dandona L. Refractive error blindness. Bull World Health Organ 2001;79:237‑43.
World Health Organization Global Data on Visual Impairment. Available from: http://WWW.WHO.int/blindnessGLOBALDATAFINALforwebpdf?ua=/fs282/en/2010. [Last accessed on2020 Mar 16].
Zhao J, Mao J, Luo R, Li F, Pokharel GP, Ellwein LB. Accuracy of noncycloplegic autorefraction in school‑age children in China. Optom Vis Sci 2004;81:49‑55.
Michaeline I, Sheriff A, Bimbo A. Paediatric refractive errors in an eye clinic in Osogbo, Nigeria. Ethiop J Health Sci 2016;26:145‑52.
Onakpoya OH, Adeoye AO. Childhood eye diseases in southwestern Nigeria: A tertiary hospital study. Clinics (Sao Paulo) 2009;64:947‑52.
Abah ER, Oladigbolu KK, Samaila E, Gani‑Ikilama A. Ocular disorders in children in Zaria children’s school. Niger J Clin Pract 2011;14:473‑6.
Adio AO, Alikor A, Awoyesuku E. Survey of pediatric ophthalmic diagnoses in a teaching hospital in Nigeria. Niger J Med 2011;20:105‑8.
Faderin MA, Ajaiyeoba AJ. Refractive errors in primary school children in Nigeria. Niger J Ophthalmol 2001;9:10‑4.
Pokharel GP, Negrel AD, Munoz SR, Ellwein LB. Refractive error study in children: Results from Mechi Zone, Nepal. Am J Ophthalmol 2000;129:436‑44.
Naidoo K, Govender P, Holden B. The uncorrected refractive error challenge. Community Eye Health 2014;27:74‑5.
Naidoo KS, Jaggernath J. Uncorrected refractive errors. Indian J Ophthalmol 2012;60:432‑7.
Xiao X, Liu WM, Ye YJ, Huang JZ, Luo WQ, Liu HT, et al. Prevalence of high astigmatism in children aged 3 to 6 years in Guangxi, China. Optom Vis Sci 2014;91:390‑6.
Adhikari S, Nepal BP, Shrestha JK, Khandekar R. Magnitude and determinants of refractive error among school children of two districts of Kathmandu, Nepal. Oman J Ophthalmol 2013;6:175‑8.
Lawan A, Eme O. Pattern of childhood refractive errors in Kano, Nigeria. Borno Med J 2018;5:1‑3.
Olusanya BA, Ugalahi MO, Ogunleye OT, Baiyeroju AM. Refractive errors among children attending a tertiary eye facility in Ibadan, Nigeria: Highlighting the need for school eye health programs. Ann Ib Postgrad Med 2019;17:49‑59.
Opubiri I, Adio A, Megbelayin E. Refractive error pattern of children south‑south Nigeria: A tertiary hospital study. Sky J Med Sci 2013;1:10‑4.
Ntim‑Amponsah CT, Ofosu‑Amaah S. Prevalence of refractive error and other eye diseases in schoolchildren in the Greater Accra region of Ghana. J Pediatr Ophthalmol Strabismus 2007;44:294‑7.
He M, Huang W, Zheng Y, Huang L, Ellwein LB. Refractive error and visual impairment in school children in rural southern China. Ophthalmology 2007;114:374‑82.
Pan CW, Klein BE, Cotch MF, Shrager S, Klein R, Folsom A, et al. Racial variations in the prevalence of refractive errors in the United States: The multi‑ethnic study of atherosclerosis. Am J Ophthalmol 2013;155:1129‑38.e1.
Rai S, Thapa HB, Sharma MK, Dhakhwa K, Karki R. The distribution of refractive errors among children attending Lumbini Eye Institute, Nepal. Nepal J Ophthalmol 2012;4:90‑5.
Biswas J, Saha I, Das D, Bandyopadhyay S, Ray B, Biswas G. Ocular morbidity among children at a tertiary eye care hospital in Kolkata, West Bengal. Indian J Public Health 2012;56:293‑6.
Villegas EA, Alcón E, Artal P. Optical quality of the eye in subjects with normal and excellent visual acuity. Invest Ophthalmol Vis Sci 2008;49:4688‑96.
Czepita D, Mojsa A, Ustianowska M, Czepita M, Lachowicz E. Role of gender in the occurrence of refractive errors. Ann Acad Med Stetin 2007;53:5‑7.
Schellini S, Ferraz F, Opromolla P, Oliveira L, Padovani C. Main visual symptoms associated to refractive errors and spectacle need in a Brazilian population. Int J Ophthalmol 2016;9:1657‑62.
Kuswanto V, Kurninwan F, Shinta AD. Association between refractive error types and asthenopia in primary school students. Majalah Kedokteran Bandung 2021;53:126‑31.
Parikshit G, Clare G. Blindness in children: A worldwide perspective. Community Eye Health 2007;20:32‑3.
Maul E, Barroso S, Munoz SR, Sperduto RD, Ellwein LB. Refractive error study in children: Results from La Florida, Chile. Am J Ophthalmol 2000;129:445‑54.
Harvey EM, Dobson V, Miller JM. Prevalence of high astigmatism, eyeglass wear, and poor visual acuity among Native American grade school children. Optom Vis Sci 2006;83:206‑12.
Nwosu SN, Alozie IU. Refractive errors in school children in Onitsha, Nigeria. Niger J Health Biomed Sci 2006;5:114‑7.
Li L, Ma Y, Hu X. A research of infant refraction in Kunming Municipality. Zhonghua Yan Ke Za Zhi 2001;37:24‑7.
Published
Issue
Section
License
Copyright (c) 2024 Journal of The Medical Women's Association of Nigeria

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.